Autoclaves are closed chambers that apply heat and sometimes pressure and steam, over a period of time to sterilize medical equipment. Autoclaves have been used for a century to sterilize medical instruments for reuse. Surgical knives and clamps, for instance, are put in autoclaves for sterilization.
For medical waste that will be disposed of, autoclaves can be used as heat treatment processing units to destroy microorganisms before disposal in a traditional landfill or further treatment. Autoclaves are a batch process, not a continuous one. Autoclaves are "chemical free" and that appeals to many stakeholders in a complex waste management environment. Chemical-free means no chemicals are added.
Autoclaves are best for wastes that are unlikely to combust or give off substantial off-gas. While incinerators can be built with pollution abatement systems, autoclaves are smaller and it is not economical to make a treatment system for vapors that evolve from the unit.
One problem with 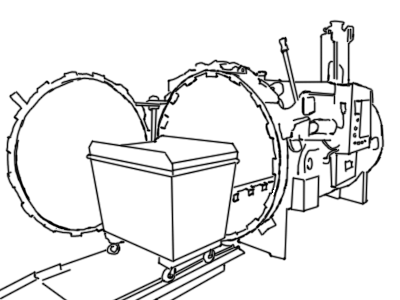 autoclaves is that the process can aerosolize chemicals present in the waste, leading to the potential for release of materials you would prefer to not release. This can pose a hazard to human operators and to some extent the environment – even though the facility HVAC system may take much of the brunt. It is possible this aerosolized material will deposit on surfaces in ductwork or countertops and floors in your facility – much as what happens in a kitchen. Aerosolized grease is the source of much grime in kitchens.
autoclaves is that the process can aerosolize chemicals present in the waste, leading to the potential for release of materials you would prefer to not release. This can pose a hazard to human operators and to some extent the environment – even though the facility HVAC system may take much of the brunt. It is possible this aerosolized material will deposit on surfaces in ductwork or countertops and floors in your facility – much as what happens in a kitchen. Aerosolized grease is the source of much grime in kitchens.
Are autoclaves a substitute for incineration? Yes, to a large extent. Autoclaves can be used to process the large bulk of infectious waste produced at a hospital or clinic. Autoclaves come in a wide range of sizes and capacities.
Big autoclaves are metal vessels in a cylindrical shape. This shape is better suited to high pressures than rectangular boxes. During operation the pressure inside the vessel is higher than the ambient pressure. There is a door on the end, and the words "auto" and "clave" mean automatic locking due to high pressure, but for safety reasons most are also sealed manually from outside.
Small autoclaves are electric - they run on the building’s power. Large ones sometimes use steam. This is convenient if the facility has steam utility. If not, a boiler must be included. Designs include autoclaves with external jackets or with internal heating pipes. Borrowing from incineration technology the word "retort" is sometimes used to refer to the autoclave chamber.
Larger autoclaves often operate under vacuum or a steam atmosphere. Pre-vacuum (or high-vacuum) autoclaves have a pump that is used to evacuate air after the chamber is sealed but before heating. Gravity-displacement autoclaves work by injecting steam into the chamber and thereby driving out the air that was present.
Operating temperature is typically 250 to 280 °F. Follow the autoclave manufacturer’s instructions and learnings from treatments of previous batches. Batch time is up to 30 minutes.
Autoclaves remind people of pressure cookers used in kitchens, and they are indeed similar. Autoclaves are basically dumb hot chambers and with a combination of time and temperature you can sterilize pretty much anything, so there is a temptation to put all sorts of medical waste in it. Autoclaves were first used (over a century ago) to sterilize medical instruments so they could be reused. When people started worrying about infectious waste they were throwing away, the autoclave was sitting there and able to accomplish disinfection/sterilization. However, putting substantial quantities of waste in autoclaves for treatment is not recommended by the community of waste management professionals. There are safer and more thorough means of treating waste.
Modern medical waste management systems incorporate autoclaves for processing of waste cultures, sharps, gauzes, bandages, and more. Sometimes surgery waste and plastic and metal waste contaminated with blood or other bodily fluids are put into autoclaves. But major treatment and any packaging for disposal must take place elsewhere.
The process design of any waste management system must consider the cycle time of the autoclave. Total cycle time includes
The cycle time of an autoclave cannot be modified. Attempts to cut corners will result in safety violations. These include violation of the time-temperature protocol for waste sterilization and opening the autoclave before it has cooled sufficiently, endangering human operators.
the autoclave before it has cooled sufficiently, endangering human operators.
Autoclaved medical waste is usually compacted after it cools down. The compaction process may include shredding before the compression. The compaction process reduces the volume of the treated waste significantly.
Periodically, operators must run tests to ensure a sufficient vacuum can be achieved before steam is introduced. The industry standard is the Bowie-Dick test which was developed a half century ago. Operators, regulators, and autoclave manufacturers know the Bowie-Dick test and its use makes things easier for managers of medical and research facilities and gives confidence the autoclave is working as intended. The autoclave manufacturer may recommend a frequency or the appropriate authority might specify how often confirmation with a spore test is required. For instance, the state of West Virginia requires a spore test every 40 hours of operation. Other experts recommend testing every day, especially if the autoclave is turned off and allowed to cool over night.
You should keep a log of autoclave activity - date, time of batch processing, what is put into the autoclave (including mass), and when you run the Bowie-Dick test and whether the autoclave passed that test. Calibration of temperature and pressure should be done in accordance with manufacturer’s recommendations and the dates and results of calibration should be recorded in the log. Even if the your state or local regulators do not require a log book, it is a good idea to keep one.
Your state or local authority may also require regular checking of the autoclave mechanics by an external and independent inspector.
Remember, the purpose of the autoclave is primarily to destroy microbes. Burning off of small amounts of combustible material may occur, especially in a dry system where there is available oxygen. But don’t put stuff in autoclaves you expect might undergo a chemical reaction in any bulk. Don’t put volatile materials in the autoclave or hazardous organic waste. And don’t expect an autoclave to have any effect on radioisotopes.
You can’t put in RCRA hazardous waste in an autoclave. You can’t put in heavy metals and expect them to be not hazardous when they come out. You could get into regulatory trouble as that would look like incineration of hazardous waste, and incinerators are subject to further air pollution and ash handling rules.
Could pathological waste - human tissue - be treated in autoclaves? No. Human and animal flesh has lower thermal conductivity than metal, so a longer time in the autoclave would be required than for surgical instruments of comparable size. There is also a concern that autoclaved pathological waste may contain low levels of radioactive material or cytotoxic compounds that have survived the heat. In any case the rules and norms in most parts of the world call for incineration of pathological waste at high temperature.
Vendors also sell hot air ovens for lab use. These are electric and do not have special venting. They can go up to 350 °F, which as hot as most autoclaves can get.
If the autoclave doesn’t reach the target temperature and maintain that temperature for the appropriate time, the process is not complete and sterilization may not occur. There are several reasons this could occur.
Some material on treatment design.
